


Your financial outcomes shouldn’t dictate your clinical workflows. It should be the other way around. Exactrx automates from clearance to claims, aligning payer policy to the way care is actually delivered. The result is fewer delays, fewer denials, and teams focused on patients, not paperwork.
Our architecture processes unstructured clinical records alongside over 80,000+ payer and guideline rules using (1) a Clinical Data Extraction Layer to structure patient records and (2) a Rules Parsing Layer to interpret criteria. It then applies (3) a Reasoning Core to generate clear, evidence-backed recommendations that show what’s needed and why.
We evaluate the documentation that already exists, use a hub-and-spoke approach to collect what’s missing, and create a complete bundle for submission through fax or other channels.
We surface what’s incomplete before cases hit the schedule, running policy and protocol checks through an API-first model to ensure patients move through and providers get paid.
We keep providers and facilities happy by cutting down the back-and-forth, requiring no training or workflow changes, since everything runs quietly in the background.
Your operations should catch gaps before they stall a case, stop downgrades before they hit revenue, and make sure providers are paid. We make that happen.
Our platform builds submission-ready pre-authorization packets automatically. We validate CPT and ICD codes against payer policies, confirm medical necessity, and bundle all supporting documentation into one complete file. The result: fewer denials, faster reimbursement, and less back-and-forth for your team.
.png)
We support pre-procedural clearance by extracting labs, consults, and authorizations from the chart, checking them against gold-standard clinical guidelines, and flagging gaps before scheduling to prevent procedural delays and denials.
.png)
The platform scans charts, validates CPT and ICD codes, applies payer-specific rules, and generates complete, submission-ready claims packets. By preventing errors, reducing denials, and speeding reimbursement, Exactrx helps claims teams and central business offices maximize revenue and efficiency.
.png)
.gif)
Exactrx automates the heavy lift of pre-procedural clinical and financial clearance. It understands complex clinical processes, parses unstructured notes, and speaks healthcare in a way that feels native because it was built with clinicians. Every recommendation is double checked by a second, more powerful model running offline. Think of it as an independent auditor: it re-analyzes patient data, cross references guidelines, and flags mismatches. By the time it reaches your team, the work is already done. Your job is simply to review and confirm.
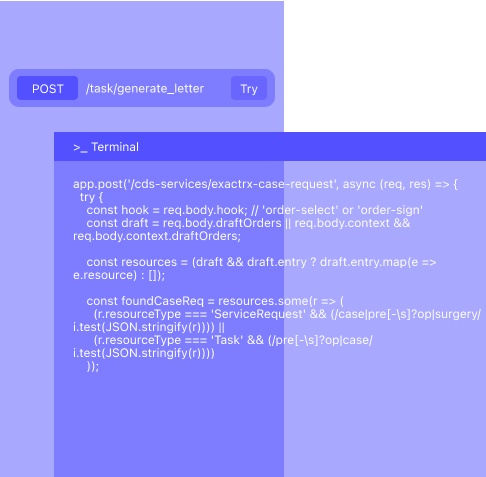
We are API-first, designed to plug directly into existing workflows. Our platform integrates with major EMRs like Epic, HST, and AthenaHealth using FHIR standards, ensuring real-time access to chart data without adding new steps for staff.





We deliver robust APIs and FHIR-First connectivity, paired with clean documentation and secure infrastructure that fits with your existing stack. Our forward-deployed clinicians and engineers work side-by-side with your teams to ensure success.
We power the most efficient care facilities.

You’ve been redirected to our new website as part of our rebranding from Celeste to ExactRx. We’re excited to introduce a stronger focus on delivering precision-driven, AI-powered healthcare solutions. Our rebrand reflects our commitment to providing more advanced, comprehensive tools for clinical efficiency and patient care.